Peroxisomal Disorders
Peroxisomal Disorders
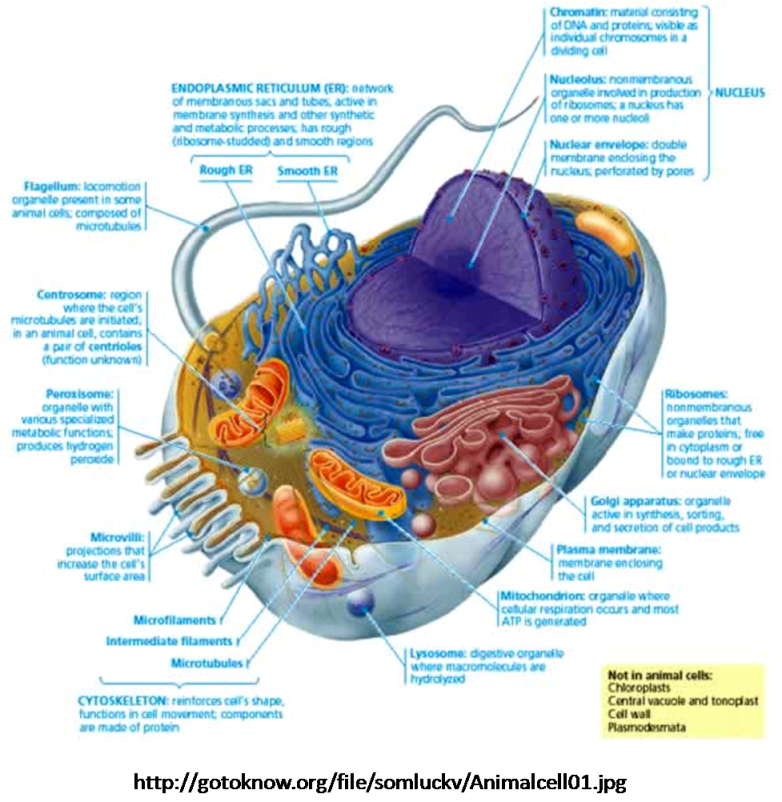
Peroxisomes are intracellular organelles that contain enzymes for β-oxidation. These enzymes overlap in function with those in mitochondria, with the exception that mitochondria lack enzymes to metabolize very long-chain fatty acids (VLCFA), those 20 to 26 carbons in length. Therefore, peroxisomal disorders generally manifest with elevated VLCFA levels (except rhizomelic chondrodysplasia). Although VLCFA levels may help screen for these disorders, other assays are also required (plasma levels of phytanic, pristanic, and pipecolic acids; RBC plasmalogen levels).
There are 2 types of peroxisomal disorders: those with defective peroxisome formation and those with defects in single peroxisomal enzymes. X-linked adrenoleukodystrophy is the most common peroxisomal disorder (incidence 1/17,000 births); all others are autosomal recessive, with a combined incidence of about 1/50,000 births.
Zellweger syndrome (ZS), neonatal adrenoleukodystrophy, and infantile Refsum’s disease (IRD): These are 3 expressions of a disease continuum, from most (ZS) to least (IRD) severe. The responsible genetic defect occurs in 1 of at least 11 genes involved in peroxisomal formation or protein import (the PEX gene family).
Manifestations include facial dysmorphism, CNS malformations, demyelination, neonatal seizures, hypotonia, hepatomegaly, cystic kidneys, short limbs with stippled epiphyses (chondrodysplasia punctata), cataracts, retinopathy, hearing deficit, psychomotor delay, and peripheral neuropathy. Diagnosis is by demonstrating elevated blood levels of VLCFA, phytanic acid, bile acid intermediates, and pipecolic acid. Experimental treatment with docosahexaenoic acid (DHA—levels of which are reduced in patients with disorders of peroxisome formation) has shown some promise.
Rhizomelic chondrodysplasia punctata: This defect of peroxisomal biogenesis is caused by PEX7 gene mutations and characterized by skeletal changes that include midface hypoplasia, strikingly short proximal limbs, frontal bossing, small nares, cataracts, ichthyosis, and profound psychomotor retardation. Vertebral clefts are also common. Diagnosis is by x-ray findings, serum elevation of phytanic acid, and low RBC plasmalogen levels; VLCFA levels are normal. There is no effective treatment.
X-linked adrenoleukodystrophy: This disorder is caused by deficiency of the peroxisomal membrane transporter ALDP, coded for by the gene ABCD1.
The cerebral form affects 40% of patients. Onset occurs between age 4 and 8 yr, and symptoms of attention deficit progress over time to severe behavioral problems; dementia; and vision, hearing, and motor deficits, causing total disability and death 2 to 3 yr after diagnosis. Milder adolescent and adult forms have also been described.
About 45% of patients have a milder form called adrenomyeloneuropathy (AMN); onset occurs in the 20s or 30s, with progressive paraparesis, and sphincter and sexual disturbance. About 1⁄3 of these patients also develop cerebral symptoms.
Patients with any form may also develop adrenal insufficiency; about 15% have isolated Addison’s disease without neurologic involvement.
Diagnosis is confirmed by isolated elevation of VLCFA. Bone marrow or stem cell transplantation may help stabilize symptoms in selected cases. Adrenal steroid replacement is needed for patients with adrenal insufficiency. Dietary supplement with a 4:1 mixture of glyceryl trioleate and glyceryl trierucate (Lorenzo’s oil) can normalize plasma VLCFA levels and may be beneficial in some cases but is under study.
Classic Refsum’s disease: Genetic deficiency of a single peroxisomal enzyme, phytanoyl-CoA hydroxylase, which catalyzes metabolism of phytanic acid (a common dietary plant component), causes phytanic acid accumulation.
Clinical manifestations include progressive peripheral neuropathy, impaired vision from retinitis pigmentosa, hearing deficit, anosmia, cardiomyopathy and conduction defects, and ichthyosis. Onset is usually in the 20s. Diagnosis is confirmed by elevation of serum phytanic acid and decreased levels of pristanic acid (phytanic acid elevation is accompanied by pristanic acid elevation in several other peroxisomal disorders).
Treatment is dietary restriction of phytanic acid (< 10 mg/day), which can be effective in preventing or delaying symptoms when started before symptom onset.
Leave a comment